Safety of biomaterials in time of coronavirus
Biomaterials resisting the pandemic.
Safety and biocompatibility are a topic of discussion when talking about biomaterials. It is always in question, particularly that of allogenic and xenogenic materials. Many doctors and patients are concerned about the current pandemic situation, which makes this argument even more relevant. Here we will write about the safety of biomaterials in times of coronavirus.
Patient information in the times of COVID-19
Although communication with the patient has always been essential for the success of the treatments, today, it is vital to clarify doubts before surgery. Many patients feel unsafe, sometimes thanks to the media, fear the possibility of infection and postpone "supposedly" unnecessary surgeries so as not to have to go to the doctor or dentist, even though this may have devastating consequences for their health.
Doctors and dentists who are successful have gained patients' trust by changing and adapting their treatments and hygiene practices to increase a sense of safety for their patients, even before the surgical procedure. In these challenging times, dental providers must implement initiatives to support the continuation of treatment. For example, during patient education, a comprehensive discussion of the origin and potential risks of animal, synthetic, or human products.
Changes in the risk analysis of biomaterials given the new regulations on medical products (MDR) and COVID-19
In the case of grafts derived from allogeneic tissue, for example, maxgraft® will change nothing even after the new regulation on medical devices (MDR) comes entirely into effect: allografts will remain within the scope and application as human tissue. This directive regulates, in particular, the donation, extraction, and testing necessary for producing these products. For Germany ( Boss biomaterials is a German company), this will mean that its approval will continue to be required under the law on medicines (historically more rigorous than the law on medical products).
Implantable materials of animal origin, synthetic materials that degrade in the body, such as some bone grafts (e.g., maxresorb®) and collagen membranes, were already classified as Class III medical devices under the previous directive (MDD). These products are subject to high regulatory requirements and safety standards; for example, in the case of products of animal origin, monitoring of zoonoses must be carried out and updated annually. Another essential measure to be followed by European companies is the monitoring of diseases that can be transmitted from animals to humans, whether they are known or newly discovered. This measure evaluates and analyses the procedures adopted to reduce or eliminate the risk of transmission (e.g., hygiene standards in the recovery of raw materials or specific measures in production to inactivate pathogens).
The transmission of possible viruses, such as SARS-CoV-2, can be excluded by measures already established for the inactivation of viruses and other pathogenic sources. For example, both high-temperature treatment of xenogenic materials such as cerabone® and treatment with ethanol and hydrogen peroxide, such as that performed for allogeneic bone grafts and collagen products from Botiss, effectively inactivate viruses, including SARS-CoV-2 virus.
The most significant changes with the introduction of MDR will be stricter clinical surveillance of medical devices after their commercialization and the introduction of more rigorous requirements in the provision of clinical evidence for Class III medical devices. In the future, it will be possible to carry out audits without prior notice and random and product testing. On the other hand, even stricter product safety and performance requirements will apply. In addition, manufacturers will be increasingly obliged to document clinical data.
For established products, almost nothing will change, as long as they are:
- The products have been on the market for a long time
- Sufficient clinical data is available in the form of studies/publications.
- A sound post-market surveillance system is in place.
Therefore, Botiss is well-positioned to meet the highest requirements even after the introduction of MDR.
Characteristics and safety of allogenic materials
Absence of a donor site and morbidity, rapid remodeling, safe supply... The advantages of allografts have convinced many users. Allogeneic bone is decellularized and sterilized, and so far, there is not a single clinical case of infection or relevant immunological reaction, such as an allergic reaction.
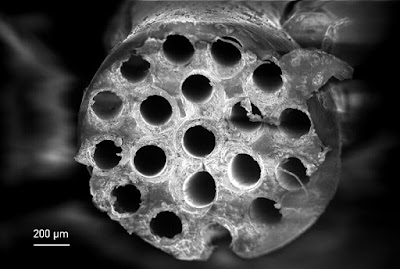
While high-temperature treatment is standard for xenogenic bone graft materials, this does not apply to allografts. The reason is that the biological value of allografts can be transferred from a human donor to another recipient without having to fundamentally change their structure and composition. This allows actual remodeling and bioabsorption for its replacement by vital bone. This quality is demonstrated, for example, in the histological studies carried out after the use of maxgraft® cancellous bone granules.
Unlike so-called "human or animal tissue derivatives," in which individual substances are isolated from the original tissues, Botiss allografts come from intact bone tissue, whether spongy, cortico-spongy, or cortical, where the natural structure and native composition of the bone are preserved, but the cellular substance is almost completely removed. This minimizes any risk of immunity, contagion, or infection.