What to do when the third molar is symptomatic?
Third molar and lower dental nerve.
There is high and sometimes controversial variability in the indication of extraction of third molars.
The ICD-10 classification (international statistical classification of diseases and health-related problems).
When the third lower molars are asymptomatic, the recommendation is clinical and radiological control by your dentist, stomatologist, or oral and maxillofacial surgeon.
When they produce symptoms such as altered tooth eruption, impacted teeth, including teeth, dental ankylosis, chronic gingivitis, and an adult paradental cyst.
The morbidity by extraction of the third lower molar is related to the age of the patient, depth of the inclusion, proximity to the more inferior dental nerve, previous treatments with radiotherapy that includes the region of the third lower molar in the field of irradiation, treatments with oral or endovenous bisphosphonates, treatment of systemic diseases with monoclonal antibodies or methotrexate.
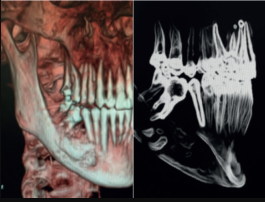
A computerized axial tomography or cone beam radiography for assessing the relationship between the lower dental nerve and the third molar improves the accuracy of the diagnosis (anatomical relationship and bone density) but does not seem to be a tool that reduces the risk of injury to the tooth.
The experience, skill, and surgical training of the dentist, stomatologist, or oral and maxillofacial surgeon does appear to be a factor that decreases the risk of lower dental nerve injury.
Lower dental nerve injury
 |
| The intimate relationship of high-risk lower third molar teeth. |
All those who perform oral surgery, oral surgery or whatever you want to call it, either in the surgical procedure of extracting the third molars or in the placement of osseointegrated implants, the possible injury of the lower dental nerve is a stressor for those who perform the surgery and the early postoperative period after the effect of the anesthetic block disappears in a few hours.
Performing a regional block of the oral, lingual, and lower dental nerves can affect these nerves. In a prospective study of patients referred with permanent alteration after a regional bloc, the percentage of patients affected by the more inferior dental nerve was 21%, and the lingual nerve was 79%. By extrapolation, the incidence of permanent lower dental and/or lingual nerve injury would be 1/26,762 to 1/160,571 procedures and regional trunk anesthesia.
Risk in the third lower molar extraction is temporary or permanent damage to the more inferior dental nerve: provisionally between 0.35-8% and permanent between 0-1% of extractions.
Injuring the lower dental nerve can lead to altered sensitivity due to excess, defect, or quality. The alterations due to quantity or rate can be without stimulus and therefore maintained constantly for 24 hours a day or after stimulating the skin by touching or rubbing it.
We speak of paresthesia when there is a sensation of itching, tingling, or prickling. By default, we speak of anesthesia when there is a total lack of sensitivity and hypesthesia when there is a partial lack of sensitivity. When it is by excess, we speak of hyperesthesia when there is a painful increase in insensitivity. More than one disorder often coexists, e.g., hypesthesia and paresthesia, usually after tactile stimulation of the skin.
Hypesthesia is usually related to a partial injury of the lower dental nerve and anesthesia to complete damage of the inferior dental nerve. While hyperesthesia and paresthesia aregeneare generallynd seem related to Wallerian degeneration.
Asymptomatic lower third molar vs. symptomatic and lower dental
In cases where the lower third molar is asymptomatic or symptomatic, where there is no close or intimate relationship with the lower third molar, it is clear: if it is asymptomatic, the general recommendation is to abstain from therapy, and if it is symptomatic, to extract the third molar.
There is most controversy in cases where the lower third molar is asymptomatic or symptomatic and in an intimate relationship between the lower tooth and the wisdom tooth;. However, most authors recommend the extraction of these third molars; the risk must be weighed.
 |
| The intimate relationship of high-risk lower first molar teeth with the cyst. |
Those who are asymptomatic need to abstain from therapy. At the same time, for those who are symptomatic and require surgery, this is based on a surgical exploration first and an evaluation of the resistance of the third molar to rule out ankylosis of the same. Crown-rThen, crown-radicularsectioning and the extraction of only the crown, if the risk is high and in the face of the impossibility of ¨botar ¨ the or the roots with an Ash 3C type pusher or Heidebrink roots, abandoning what a French Oral and Maxillofacial Surgeon called "the technique of usury."
This situation requires annual clinical and radiological controls with periapical radiography between two and five years.
The annual radiological controls during five years, for the third symptomatic inferior molars as the abandonment of the root or roots of the same one in the "Technique of the usury," are the criterion of consensus.
 |
| Usury technique on first lower molar, cystectomy, and guided bone regeneration |
Evidence-based medicine. Basis of Usury Technique on the Lower Third Molar.
It is based on clinical and radiological observation in patients who carry "well-tolerated" root remains both in their bone beds and in their gum lining, which allows us to think about this action to avoid injury to the lower dental nerve in high-risk situations. Also, in findings in prehistoric jaws, root remains that have not given rise to bone lesions are "well-tolerated."
The "usury technique" can be extended to other dental pieces with a high risk of injury to the lower teeth. Possible complications after thyroidectomy are migration, mobility, or root eruption. Guided bone regeneration can be performed together with thyroidectomy.
It must always be accompanied by adequate information to the patient with the consequent informed consent in which the possible abandonment of the root is recorded.
Summary
The indication for the extraction of third molars, in general, is often made lightly by the dentist, stomatologist, or oral and maxillofacial surgeon, and even more so when they are not going to be the ones to perform the surgical extraction.
The appropriate clinical and radiological evaluation associated with the experience of the dentist, stomatologist, or oral and maxillofacial surgeon are the fundamental factors in preventing lower dental injury by adapting the risk to the benefit.
In the era of evidence-based medicine, thyroidectomy or "usury technique," with or without guided bone regeneration, is an efficient method in preventing lower dental nerve injury in the teeth included, where the probability of occurrence is high, is an option to be explained to the patient.
