Central Sleep Apnea
Obstructive Sleep Apnea Syndrome.
 |
| Pediatric Patient with Severe Obstructive Sleep Apnea Syndrome |
Current evidence supports the association between the upper airway and craniofacial anatomy. As extracted from this article, anatomical features are associated with greater collapsibility of the pharyngeal space during sleep. Given the implementation of 3D imaging studies in dental practices, detailed analysis of the upper airway in patients can be helpful for early disease detection. However, more extensive and perfectly protocolized image studies are needed to confirm this relationship between anatomy and Obstructive Sleep Apnea Syndrome.
However, more extensive and perfectly protocolized image studies are needed to confirm this relationship between anatomy and Obstructive Sleep Apnea Syndrome.
Introduction
Obstructive Sleep Apnea Syndrome is a common condition that can occur at any age, even in young children. Its prevalence has been estimated in recent studies in 24% of males and 9% of females and in 2-4% of the pediatric population.
One of the problems related to this disease is underdiagnosis; it is estimated that only 9% of patients are diagnosed. Symptoms such as chronic fatigue, daytime sleepiness, snoring associated or not with aspheric episodes, arterial hypertension, or depression refractory to adequate treatment should alert us. In children, the first warning sign is often the existence of attention deficit, hyperactivity, or poor school performance. Obesity seems to be a consequence of the diseas ands a risk factor, but it is not a constant in all cases.
Obstructive Sleep Apnea Syndrome is characterized by apnea or hypopnea pauses during sleep. Repeating these pauses throughout the night produces intermittent hypoxemia, as the drop of oxygen in the blood causes micro awakenings that restore ventilation but prevent restorative sleep. The consequence of this situation is daytime sleepiness and chronic fatigue, which are related to increased traffic accidents and accidents at work and home. It is, therefore, a significant public health problem.
In addition, and due to complex etiopathogenic mechanisms, this disease is related to an increase in the incidence of cardiovascular, vascular brain, metabolic, type II diabetes, obesity and E.T.S. (refractory to conventional treatment), depression, impotence, decreased libido, lack of concentration, headaches and has even been related to cancer and sudden death, both in children and adults. Therefore, early diagnosis is vital in the pediatric patient, as the disease can impede normal physical and intellectual development.
Craniofacial Growth and Airway
Jared Diamond, an American researcher at U.C.L.A., enunciated a hypothesis he called "A Great Leap Forward. This theory explains how the respiratory tract of modern Homo Sapiens evolved for speech acquisition. Based on this hypothesis, he considers O.S.A. to be an adverse effect of this evolution due to changes in the anatomy of the respiratory tract. These anatomical changes in the bones of the skull and face have placed him in a situation more prone to Obstructive Sleep Apnea Syndrome.
According to this theory, the bones of the face experienced, during evolution, a rearward movement; the mandible followed the maxilla rotating down and back, flattening the face; the soft palate and ethmoids shortened. The tongue was thus retroposition to occupy a part of the oral cavity and another in the oropharynx. As a result, the size of the language did not involute like that of the jaws, maintaining its proportions. In addition, the angulation of the base of the skull became greater. The larynx descended and was placed approximately at the level of the fourth cervical vertebra. The foramen Magno was placed in a more advanced position, reducing the space available for the pharynx. These changes in the craniofacial skeleton would cause the soft tissues to be positioned in a way that can more easily obstruct the airway during sleep. The descent of the larynx has made the airway longer, curved, narrower, and, therefore, more collapsible.
A facial cranium disharmony in an individual (child or adult) may be a predisposing factor to Obstructive Sleep Apnea Syndrome since the anatomical relationship between skeletal structures and soft tissues will determine the permeability of the airway. Structurally, the pharynx can be considered a soft tissue tube surrounded by a bone framework: cranial base, vertebral column, nasal septum, maxillary and hiodic bone. The tension and size of the soft tissues will, in turn, be related to the size and position of the hard tissues that contribute to the shape and dimensions of the upper airway. In this way, the morphological and dimensional characteristics of the VAS will change with the growth of the craniofacial hard and soft tissues.
Many authors have investigated the possible relationship between respiratory patterns and the airway with craniofacial morphology and malocclusion development. Despite many articles on respiration, facial cranium deformities, and Obstructive Sleep Apnea Syndrome, the exact relationship between them remains unknown. While some authors establish an association between facial cranium disharmony and sleep disorders, others refute this relationship. It is pointed out that alterations in breathing (function), such as those due to an obstructive disorder, can generate changes in the facial cranium bone structure, the jaws, and the tongue and even produce changes in the posture of the head. A frequent respiratory dysfunction or a deviation in the nasal septum could cause a decreased nasal flow, a change from a nasal to an oral pattern, and the consequent appearance of anatomical compensations such as a compressed maxilla, a lower position of the tongue, an extension of the neck or mandibular posturing. This same author states that from birth, there is a continuous and complex interaction between oro-nasal functions (breathing, sucking, swallowing, chewing) and orofacial growth. It establishes that if there are functional anomalies in the first stages of life, the risk of suffering anatomical changes in the bone structures will be increased. Therefore, the risk of collapse, especially during sleep, will be greater.
In the same line, it is evident that changes in a normal nasal breathing pattern during active growth can affect the development of the craniofacial skeleton. For example, the anteroposterior dimension of the VAS has been shown to have a proportional relationship with jaw growth and facial growth pattern. A small jaw and jaw with clockwise facial growth will result in a poor airway. It also states that severely decreased nasal flow can induce the appearance of anatomical compensations at the face and neck and have consequences on the occlusion. Structural modifications as a consequence of an alteration in the respiratory pattern may include a postponement of the mandible, lack of lip seal, increased interocclusal space, an increased anterior facial height, a lower position of the diode bone, a more forward or lower position of the tongue, change of a breathing pattern from nasal to oral, an anterior extension of the head and neck, an increase in the angle of the mandibular plane, an increase in the angle of the occlusal plane, maxillary compression, a posterior crossbite, a class II occlusion, and a clockwise growth pattern, among others. He considers that when there is an aberrant growth pattern, the final result may lead to the appearance of a phenotype known to doctors and dentists as "facies adenoidal."
Diagnostic imaging in Obstructive Sleep Apnea Syndrome
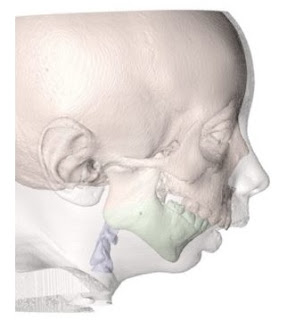
The golden standard in the diagnosis of Obstructive Sleep Apnea/Hypopnea (S.A.H.S.) is nocturnal hospital polysomnography (P.S.G.). However, despite the multiple channels of information it provides, this test does not make it possible to visualize in which anatomical region(s) an upper airway obstruction (UAV) may take place. The birth of three-dimensional (3D) technology using computed tomography (C.T.), Cone Beam (C.B.C.T.), or magnetic resonance imaging (M.R.I.), as well as the use of specialized software, has made it possible to carry out a thorough analysis of the upper airway (VAS) in recent years. These programs make it possible to calculate semi-automatically the parameters that most affect the airway: its length, total volume, area, and minimum cross-sectional area with its anteroposterior and lateral dimensions.
For both C.T. and M.R.I., the patient is supine during the test, but for C.B.C.T., the patient will remain seated. C.B.C.T. requires less radiation than C.T. and can be used in adult and child patients. For Hatcher, C.B.C.T., compared to C.T., has a favorable risk/benefit ratio for many facial cranium applications, including acquiring 3D images of the airway and its associated structures. C.T. implies a higher cost and radiation, so it would be reserved for patients undergoing surgery and/or presenting severe craniofacial malformations. For some years now, in daily dental practice, dentists have been incorporating C.B.C.T. machines into their practices, thanks to the fact that these machines are relatively small and affordable (more than a C.T. scan).
Imaging tests complement medical history, a physical examination, and, of course, a night-time hospital P.S.G. Other tests also used in S.A.H.S. are nasopharyngoscopy and D.I.S.E. (Drug-Induced Sleep Endoscopy), among others.
Since the early years of the S.A.H.S. study by radiographic techniques, lateral cranial teleradiography (T.L.C.) has been used because it is an accessible, simple to interpret, reproducible, and economical method, but it has the main disadvantage that it provides a two-dimensional image that does not represent the anatomy as it exists in nature. Moreover, being a test that is not performed during sleep can also not allow an analysis of the axial plane that is truly perpendicular to the flow of air and would oppose its passage or evaluate volumetric changes produced in the airway.
For reasons such as greater accuracy in reproducing the airway in a real way, without overlapping, and its ability to measure volumetric changes, 3D diagnostic methods are considered superior to T.L.C.
Among the radiographic methods, C.T. and C.B.C.T. are available, but it must be taken into account that the patient's position during image acquisition differs (supine decubitus or seated). Gravity will have a greater effect on airway tissues when the patient is lying down, generating volumetric differences between studies using C.T. or C.B.C.T.
